You walk into the kitchen and pause. Why did you come in here? The thought that brought you here seconds ago has vanished.
Or you’re introducing a friend and suddenly can’t recall their name—someone you’ve known for years.
Your heart skips. Is this normal, or is this the beginning of something serious?
If you’ve had that moment of fear, you’re not alone. Nearly everyone over 60 has worried whether a memory slip means something more.
The uncertainty can be exhausting—analyzing every forgotten word, every misplaced item, wondering if this is just aging or the start of cognitive decline.
Here’s what matters: there are clear, recognizable differences between normal age-related memory changes and warning signs that deserve medical attention.
Knowing these differences won’t just reduce your anxiety—it will help you monitor your cognitive health with confidence and take action when it’s truly needed.
The Memory Tracking Checklist: Know When to Seek Help
Track your memory patterns over two weeks with this simple checklist to confidently distinguish between normal aging and changes that deserve medical attention—so you can stop second-guessing yourself and get answers.
What Normal Age-Related Memory Changes Actually Look Like
Your brain at 70 processes information differently than it did at 30, but that doesn’t mean it’s failing. Certain memory changes are completely normal and expected as we age.
These are typical:
• Occasionally struggling to find the right word, especially names
• Temporarily forgetting why you entered a room
• Misplacing your keys but retracing your steps to find them
• Taking longer to learn something new, but remembering it once you do
• Needing to write things down more than you used to
• Drawing a blank on a neighbor’s name, then remembering it an hour later
These happen because processing speed naturally slows with age. Think of it like this: your knowledge and wisdom remain intact—you just access them a bit more slowly. It’s similar to needing reading glasses. Your eyes haven’t failed; they just work differently now.
I’ve worked with thousands of older adults over 20 years, and I can tell you that the sharpest, most cognitively healthy seniors I know use memory aids constantly.
They keep detailed calendars. They make lists. They set phone reminders. These aren’t signs of decline—they’re strategic tools that smart people use to work with their changing brains, not against them.
If you’re occasionally forgetting a word or where you put something, but you can retrace your steps or the information comes back to you later, your brain is functioning normally. Understanding that these changes are typical can help reduce the anxiety many people feel about aging.

The Memory Changes That Deserve Your Attention
Some memory changes are qualitatively different from normal aging. They don’t just slow down your recall—they interfere with how you store and retrieve information.
Watch for these patterns:
• Getting lost in familiar neighborhoods or places you’ve been many times
• Losing track mid-conversation or struggling to follow what people are saying
• Forgetting recent events or conversations entirely—not just the details, but that they happened at all
• Asking the same question multiple times within minutes or hours
• Having trouble with familiar tasks you’ve done for years, like following a recipe you know by heart or managing bills you’ve always handled
• Making decisions that seem out of character or show poor judgment
• Withdrawing from social activities because memory problems make them uncomfortable
Here’s a key distinction: If you forgot you had lunch with a friend yesterday, that’s potentially concerning. If you remember the lunch but can’t recall what you ate, that’s normal.
If you keep asking your daughter when she’s visiting, even though she’s told you three times this morning, that’s different from forgetting once. If you can’t remember how to make your signature dish that you’ve cooked hundreds of times, that’s not the same as forgetting where you put the recipe card.
These changes aren’t just ‘senior moments.’ They represent alterations in how your brain stores and accesses information. If you or people close to you notice these patterns, documentation becomes important. Keep a simple log with dates and specific examples of what happened.
Taking these warning signs seriously while maintaining your independence requires a balanced approach that respects both safety and autonomy.

The ABCS Method: A Framework for Monitoring Changes
When memory concerns arise, having a systematic way to track them helps distinguish between isolated incidents and meaningful patterns.
Use these four domains to monitor changes:
Activities
Can you still complete familiar daily tasks? This includes cooking meals you’ve made before, managing your finances, keeping up with hobbies, maintaining your home, and handling your medications.
Changes here might look like: burning food you’ve cooked for decades, overdrawing your checking account when you’ve always balanced it carefully, or losing interest in activities you used to enjoy not because you don’t want to do them, but because they’ve become confusing.
Behavior
Have you noticed personality shifts, increased confusion about time or place, or changes in mood? Are you more irritable, anxious, or depressed than usual?
This might show up as: suspecting people of stealing things you’ve misplaced, dramatic mood swings that are new for you, or withdrawing from social situations you used to enjoy.
Concerned about cognitive health as you age? Subscribe to our newsletter for practical strategies and expert guidance on maintaining brain health, recognizing warning signs, and supporting independence through every stage of aging.
Communication
Are you having more difficulty finding words, following conversations, or expressing your thoughts? Can people understand you as easily as before?
Warning signs include: frequently stopping mid-sentence because you can’t find words, having trouble following TV shows or conversations you could follow before, or people often asking you to repeat yourself because what you said didn’t make sense.
Safety
Are you making unsafe decisions? This includes wandering or getting lost, leaving the stove on, neglecting personal hygiene in ways that are new for you, or making financial decisions that put you at risk.
This isn’t about one incident of leaving the stove on once. It’s about patterns—repeatedly leaving the stove on, getting lost driving to places you’ve been going for years, or falling for scams when you’ve always been savvy about money.
If you’re noticing changes in just one of these areas, pay attention but don’t panic. If you’re seeing changes across multiple ABCS categories, or if any single area is showing significant change or progression, schedule a medical evaluation.
The beauty of this framework is that it prevents you from either obsessing over every small thing or dismissing legitimate concerns. You’re not catastrophizing one forgotten name—you’re looking at patterns across different aspects of daily life.
Creating systems to support your cognitive health can help you maintain independence while addressing real concerns.

When Others Notice Before You Do: The ‘Concerned Observer’ Rule
Here’s an uncomfortable truth: certain types of cognitive changes can affect your ability to accurately assess your own memory and thinking.
If multiple people in your life—your spouse, your adult children, close friends—are expressing concern about your memory or cognitive function, take that seriously even if you don’t see the problems they’re describing.
This isn’t about letting others control your life. It’s about recognizing that self-awareness can become less reliable with some cognitive conditions. The people who know you well can often see patterns you might miss.
Also pay attention to timing:
Gradual changes deserve evaluation but aren’t emergencies. If your memory has been slowly declining over months or years, schedule an appointment with your doctor in the next few weeks.
Sudden changes require urgent evaluation. If memory problems, confusion, or personality changes develop rapidly—over days or weeks—that needs immediate medical attention. Sudden cognitive changes can signal strokes, infections, medication reactions, or other treatable conditions.
The value of early evaluation:
Getting assessed early when concerns first arise provides significant advantages. You have more treatment options when conditions are caught early. You have time to plan and make decisions while you’re still able to participate fully. And many memory problems have reversible causes.
Medication side effects, vitamin B12 deficiency, thyroid problems, depression, sleep apnea, and chronic dehydration can all cause memory problems that improve with treatment.
I’ve seen people and their families agonize over ‘dementia’ symptoms that turned out to be a B12 deficiency or a medication interaction—conditions that improved dramatically with simple interventions.
During a cognitive evaluation, your doctor will likely conduct memory and thinking tests, review your complete medical history and current medications, and possibly order blood tests or brain imaging. These evaluations are thorough, but they’re not frightening. They’re designed to identify what’s happening and what can be done about it.
Seeking evaluation isn’t admitting defeat. It’s taking charge of your health with the same wisdom you’ve applied to every other challenge in your life. Understanding when to ask for help is a sign of strength, not weakness.
How to Track Changes Without Driving Yourself Crazy
Documentation serves two purposes: it gives you and your doctor concrete information to work with, and it helps you distinguish between ‘I think things are getting worse’ and ‘things are objectively changing.’
Memory concerns affect memory of concerns. You might forget incidents of forgetting, or you might remember every tiny slip because you’re anxious. Written records eliminate that guesswork.
Here’s a simple tracking format:
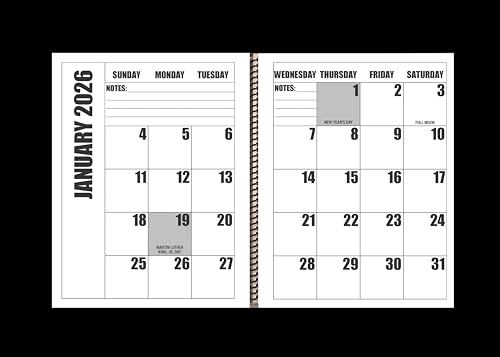
Date | What happened | Who noticed | Context
For example:
3/15 | Asked Susan when she’s visiting three times in one morning | Susan | She’d already told me twice
Or:
3/18 | Couldn’t remember if I took my blood pressure medication | Me | Morning routine
Track specific domains that matter for daily life:
• Medication management: Are you taking medications correctly, missing doses, or forgetting whether you’ve taken them?
• Appointments: Are you remembering appointments, or do you need reminders? Are you missing appointments you used to keep?
• Familiar tasks: Can you complete tasks you’ve always done—cooking, paying bills, using technology you’re familiar with?
• Conversations: Are you able to follow conversations, or do you frequently lose track of what people are saying?
How to present information to your doctor:
Bring your log to appointments. Doctors can’t observe memory problems during a 15-minute visit, but they can evaluate patterns documented over weeks. Be specific: ‘I’m having memory problems’ is vague. ‘In the last month, I’ve gotten lost driving to the grocery store twice, and I forgot my grandson’s name three times’ gives your doctor concrete information to work with.
The difference between helpful tracking and anxious over-monitoring:
Helpful tracking is noting incidents when they happen or setting aside five minutes at the end of each day to record anything noteworthy. You’re documenting, not dwelling.
Anxious over-monitoring is analyzing every thought, testing yourself constantly, or asking others to quiz you on your memory. That creates stress, which ironically can worsen memory performance.
If you find yourself obsessing over tracking, pull back. Document obvious incidents, but don’t make memory monitoring your full-time job. Managing stress is important for cognitive health, so balance awareness with peace of mind.
Some people find that using a simple memory journal, a calendar app with notes features, or a medication tracking app helps create documentation that makes conversations with healthcare providers more productive and less stressful.
The Memory Tracking Checklist: Know When to Seek Help
Track your memory patterns over two weeks with this simple checklist to confidently distinguish between normal aging and changes that deserve medical attention—so you can stop second-guessing yourself and get answers.

Moving Forward With Clarity and Confidence
Understanding the difference between normal memory changes and warning signs doesn’t eliminate the fear entirely. But it transforms vague anxiety into informed awareness.
You now know that occasional forgetfulness is normal. You know which patterns deserve medical attention. You have a framework for monitoring changes systematically. And you understand that seeking evaluation is wise, not alarmist.
If memory changes are causing you worry—even if you’re not sure they meet the ‘concerning’ criteria—that worry itself is reason enough to talk with your doctor. Persistent anxiety about cognitive function affects your quality of life, and your doctor can help you sort out what’s happening and what, if anything, needs to be done.
Early evaluation often provides relief. Many people discover their memory concerns are normal aging, medication side effects, or treatable conditions. Even when the news is more serious, early diagnosis provides time to plan, access treatments, and make decisions while you’re fully able to participate.
Trust what you’re noticing. Trust what people who know you well are noticing. You’ve navigated challenges your entire life with wisdom and good judgment. This is no different. The same qualities that have served you well until now—the ability to gather information, assess situations clearly, and take appropriate action—will serve you well here too.
Taking charge of your health in every area of your life means addressing concerns proactively while maintaining the independence and dignity you’ve earned.
Have you experienced memory changes that concerned you? What helped you decide whether to seek evaluation? Share your experience in the comments—your story might help someone else find the clarity they need.

![Older couple sofa adult child support[1]](https://www.grayingwithgrace.com/wp-content/uploads/2026/02/older_couple_sofa_adult_child_support1-e1771334039968.jpg)












![Older couple pottery wheel studio[1]](https://www.grayingwithgrace.com/wp-content/uploads/2026/02/older_couple_pottery_wheel_studio1-e1771334326831-450x300.jpg)
![Older woman side sleeping position peaceful[1]](https://www.grayingwithgrace.com/wp-content/uploads/2026/02/older_woman_side_sleeping_position_peaceful1-e1771333748525-450x300.jpg)
![Older woman evening reset coffee table[1]](https://www.grayingwithgrace.com/wp-content/uploads/2026/02/older_woman_evening_reset_coffee_table1-e1771333481812-450x300.jpg)
![Elderly woman high contrast controls microwave[1]](https://www.grayingwithgrace.com/wp-content/uploads/2025/12/elderly_woman_high_contrast_controls_microwave1-e1765217272116-450x300.jpg)
![Older black couple transcribing home office[1]](https://www.grayingwithgrace.com/wp-content/uploads/2025/11/older_black_couple_transcribing_home_office1-e1763400682707-450x300.jpg)
![Senior woman setting boundaries holiday table[1]](https://www.grayingwithgrace.com/wp-content/uploads/2025/11/senior_woman_setting_boundaries_holiday_table1-e1762888071788-450x300.jpg)
![Caregiver demo bedside fall mat[1]](https://www.grayingwithgrace.com/wp-content/uploads/2025/07/caregiver_demo_bedside_fall_mat1-e1752698516109-450x300.jpg)
![Older woman cane colorful plate divider[1]](https://www.grayingwithgrace.com/wp-content/uploads/2025/07/older_woman_cane_colorful_plate_divider1-e1752686358595-450x300.jpg)



